
Vaccine implementation might benefit from a nudge or two…
FAGLIG ORIENTERING
Af Simon Tulloch, chefkonsulent, psykolog, Dansk Selskab for Patientsikkerhed
When the historians summarise 2020 as a chapter in a book, it is likely that it will end with a cliff-hanger; on the horizon are various COVID-19 vaccines which will likely help return our lives back to normality. But how will this next phase of our COVID-19 experience go? As I write this (early December) the situation is changing on a daily basis, however, various government and news outlets are providing excellent information to help citizens understand and prepare for what will happen in terms of vaccine roll-out and implementation.

In a recent interview, Søren Brostrøm (director of the National Board of Health) said:
“It is a big task, but we have lots of experience from, for example, the child vaccination program, seasonal flu vaccination and the vaccination efforts during the pandemic in 2009. But it is clear that the task of making a plan for vaccination against COVID-19, with probably several different types of vaccines, for different groups of people, will be bigger than anything we have tried before”. (1)
Vaccinen kommer tættere på, men nogle danskere tvivler fortsat – artikel i DR
With this in mind, I was pleased to see an article in this week’s Economist magazine by Professor Catherine Milkman (2) which focuses on how behavioural sciences can help with this challenge. In the article, Milkman writes that although effective vaccines will help bring an end to COVID-19:
“society faces a new crisis: uptake. If too few people agree to get immunised, the value of a vaccine will be limited—and the world could face a situation much like today’s, with many ill and dying, social isolation and withering economies.”
In the article, Milkman refers to a recent Ipsos survey (3) which sampled people from 15 countries (not including Denmark), of which approximately three-quarters said they will get vaccinated. This number is large enough to establish ‘herd immunity’, however, this group includes 33% who ‘strongly agree’ that they will get immunised, and 40% who ‘somewhat agree’ to immunisation. Milkman suggests this latter group may need some ‘nudging’, and this is where behavioural science can be useful.
Milkman highlights two main problems for vaccine implementation with this group, firstly, the ‘persuasion problem’ and secondly the ‘follow-through problem’. In terms of ‘persuading’ people, Milkman suggests that
“Relying on information, transparency and encouragement is only the start… ‘Social proof’ also needs to be part of the effort.”
Milkman refers to research which shows that people look to their peers (4) for cues about how to behave, affecting everything from how they vote to how they save money. In Denmark, the HOPE Project (5) provides valuable data (data below) regarding how people have behaved during the Covid-19 crisis. Although these data indicate that Danes may well be more compliant with some behaviour change (hand washing) they are less so in others (avoiding crowds) than many other countries, however, this may well be (in part) due to social proof*. As such, health authorities should emphasise the wide support for vaccinations rather than focusing on naysayers. Public-service messages highlighting the popularity of the vaccine should not only be accurate but should increase demand. To supplement this approach, Milkman suggests that ‘visible markers’ may also be useful, similar to the “I Voted” stickers that Americans receive at the polls. These act as small rewards for doing one’s civic duty, but they’re also advertisements that can spur others to follow suit.
Regarding the ‘follow-through’ problem, Milkman refers to research which indicates that
“anywhere from a third to two-thirds of people (6) who say they’ll do something, such as get a medical check-up or exercise, fail to act on their intention”.
It is unlikely that people will behave any differently even for a vaccine during a pandemic. To make matters worse, the most promising vaccines, from Pfizer, Moderna and AstraZeneca, will not be “one-and-done”. Instead, they will require people to get two inoculations several weeks apart. This dramatically increases the risk of follow-through problems. If the groundwork isn’t right, many people will get the first shot but not the second. Milkman summarises a range of simple interventions which will likely make a difference, such as text-message reminders, ensuring the process is convenient (e.g. at your place of work,) and ‘hassle-free’ (i.e. no paperwork or waiting).
There are of course a range of ‘novel’ ideas to support successful implementation of the vaccine, for example, the economist and Nobel laureate Richard Thaler has suggested giving everyone who gets immunised a lottery ticket (which should feel more like a prize than a payment). By contrast, Robert Litan, a senior fellow at the Brookings Institution who served in the Bill Clinton administration, designed a plan (7) which included simply paying people $1,000.
Not surprisingly, a proliferation of documents with ‘guiding principles’ have been developed in recent weeks, two of note are the World Health Organization ‘Behavioural considerations for acceptance and uptake of COVID-19 vaccines: WHO technical advisory group on behavioural insights and sciences for health’ (8). This report was developed by international experts in behavioural economics, chaired by Cass Sustain (co-author of ‘Nudge’). A shorter read, but equally helpful is article by Kevin Volpp and colleagues titled ‘Behaviorally Informed Strategies for a National COVID-19 Vaccine Promotion Program’ (9) which provides a number of behavioural tips and tricks to support the immunisation process. Either way, Professor Milkman concludes her article by suggesting that national health authorities need to think both carefully and creatively when planning the vaccine implementation:
“The biochemists have done their part. It’s now time for the work of behavioural scientists to move the needle.”
*HOPE Project data – Comparative data of six nations regarding compliant behaviour
(data bringes med med tilladelse fra HOPE-projektet)
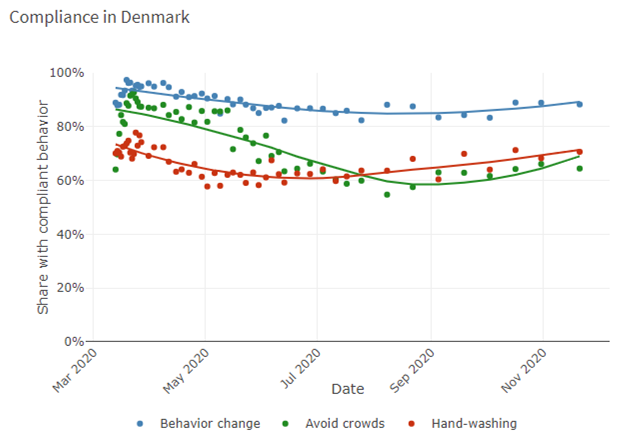
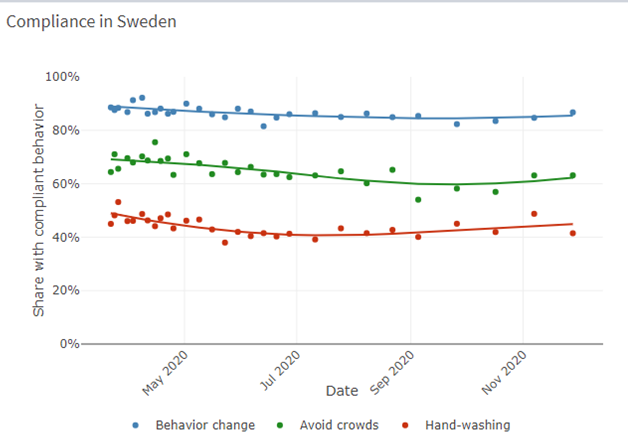
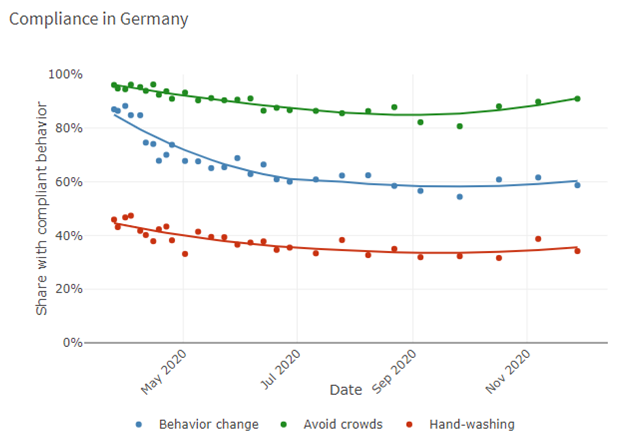
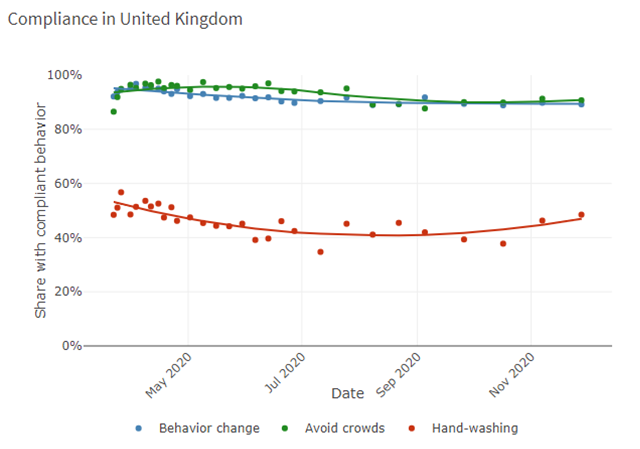
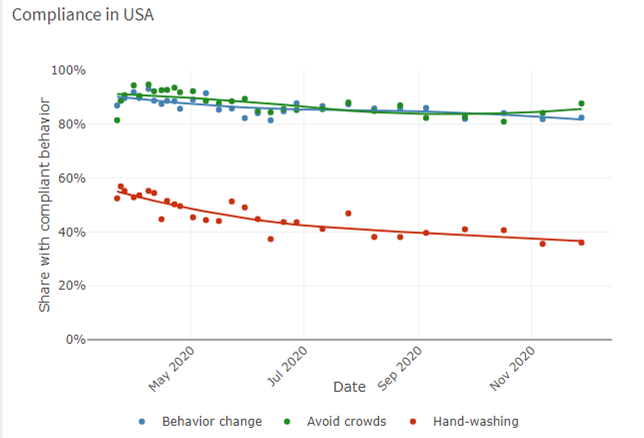
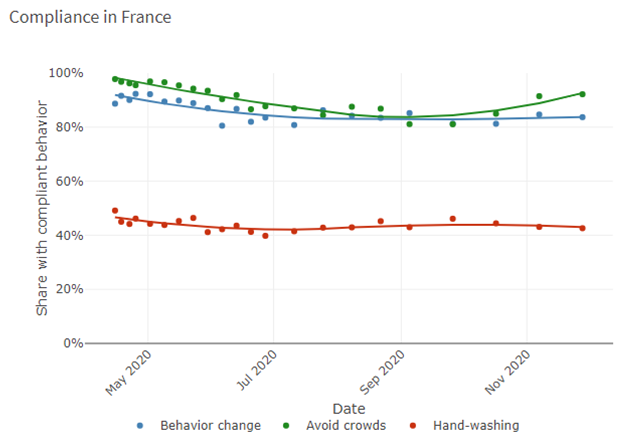
(Data accessed from: https://hope-project.dk/dashboard/ on 02.12.20)
References and useful resources:
- https://www.sst.dk/da/Nyheder/2020/Planlaegningsgrundlaget-for-den-foerste-fase-af-vaccination-mod-COVID-19-er-klar
- https://www.economist.com/by-invitation/2020/11/30/katy-milkman-on-how-to-nudge-people-to-accept-a-covid-19-vaccine
- https://www.ipsos.com/en/global-attitudes-covid-19-vaccine-october-2020
- https://www.jsmf.org/meetings/2008/july/social%20norms%20Cialdini.pdf
- https://hope-project.dk/#/
- https://www.tandfonline.com/doi/abs/10.1080/14792772143000003
- https://www.brookings.edu/opinions/want-herd-immunity-pay-people-to-take-the-vaccine/
- https://apps.who.int/iris/handle/10665/337335
- https://jamanetwork.com/journals/jama/fullarticle/2774381
- https://www.dr.dk/nyheder/webfeature/jagten-paa-vaccinen-mod-corona
- https://laegemiddelstyrelsen.dk/en/news/themes/new-coronavirus-covid-19/-vaccines-and-medicines-against-covid-19/
- https://www.sst.dk/da/corona/COVID-19-og-ny-coronavirus/Vaccination-mod-COVID-19
- https://www.businessinsider.com/covid-19-vaccine-payment-economists-stimulus-recovery-coronavirus-aid-2020-11?r=US&IR=T

Fagligt Nyt om patientsikkerhed er et nyhedsbrev, der udgives af Dansk Selskab for Patientsikkerhed, PS!, og udkommer 6 gange årligt. Det formidler nyt om de seneste nationale og internationale forskningsresultater, begivenheder, trends og meninger inden for patientsikkerhed. Mere Fagligt Nyt

